Researchers from Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago have developed artificial intelligence (AI) models that can predict the risk of sepsis in children within 48 hours, using data collected in the first four hours after a child arrives at an emergency department.
Sepsis is a severe infection that leads to life-threatening organ dysfunction and remains a leading cause of death among children globally. The study, which will be published in JAMA Pediatrics on October 13, is the first to use AI models based on the Phoenix Sepsis Criteria for pediatric patients. Previous attempts using predictive models had not succeeded in improving early diagnosis for this condition.
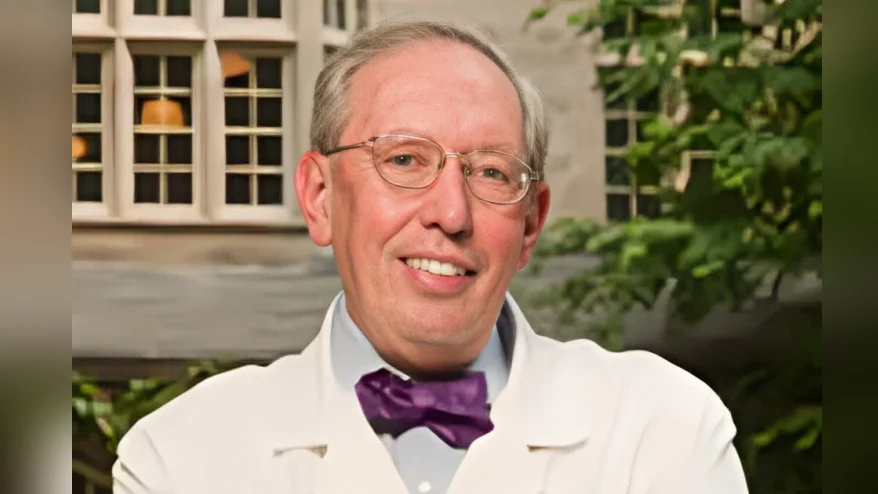
“The predictive models we developed are a huge step toward precision medicine for sepsis in children,” said Dr. Elizabeth Alpern, professor of pediatrics at Northwestern University Feinberg School of Medicine and division head of emergency medicine at Lurie Children’s. “These models showed robust balance in identifying children in the emergency department who will later develop sepsis, without overidentifying those who are not at risk. This is very important because we want to avoid aggressive treatment for children who don’t need it.”
The research analyzed routine electronic health record (EHR) data, such as triage scores, heart rate or respiratory rate, and pre-existing medical conditions like cancer. The study involved five health systems participating in the Pediatric Emergency Care Applied Research Network (PECARN), which provided access to a large and diverse dataset. Researchers examined retrospective data from January 2016 to February 2020 to develop the AI models and then validated them using data from 2021 to 2022.
Children who already had sepsis upon arrival or within the first hours of care were excluded from the study. The aim was to identify patients at risk before organ dysfunction began, allowing for early interventions that could save lives.
“We evaluated our models to ensure that there were no biases,” Alpern stated. “Future research will need to combine EHR-based AI models with clinician judgment to make even better predictions.”
The project received support from the National Institute of Child Health and Human Development (NICHD) through grant R01HD087363.